Belief and trust barriers to using digital health services: learning from a research and co-design project
More health services moving online. With funding through the VCSE Health and Wellbeing Alliance, we conducted a research and co-design project to develop a resource to help address belief and trust barriers to using digital health services.
With more and more health services moving online, there are concerns that people who face digital barriers will find it more difficult to access care. People’s beliefs and perceptions around digital health services will shape their willingness to engage with these services, with implications for their ability to access timely and appropriate healthcare.
With funding through the VCSE Health and Wellbeing Alliance, we conducted a research and co-design project to develop a resource to help address belief and trust barriers to using digital health services. Working with people with lived experience of digital exclusion, we developed a leaflet to prompt discussion of common concerns, to help people feel more confident to make choices around digital health services. The leaflet can be accessed and downloaded from our website.
Below we summarise the process and key learnings from the research and co-design project. For the full report, please download the PDF version linked in the Downloads section.
You can also watch our on-demand webinar where we talk about the insights from this research and how they can addressed.
Contextback to top
Access to health services is increasingly moving online, with opportunities for improved communication between professionals and patients, and to enable quicker, easier access to care when people need it. However, there are implications for access to care among those people facing barriers to digital inclusion. These barriers include limited digital skills and confidence, connectivity or access to a digital device. With the ‘digital front door’ being increasingly promoted, particularly across primary care, there are concerns about people’s ability to access the care they need.
Some of those who struggle to get online also face health inequalities¹, which are at risk of being compounded by increased digitisation of health services. For example, only 76% of people with an impairment have basic digital skills compared with 91% of the general population².
Even with digital skills and access in place, people can feel reluctant and concerned about using digital health services. The NHS Framework for Inclusive Digital Health Services³ identifies beliefs and trust as one of five core dimensions of ensuring accessible and inclusive digital health services. Yet, the Framework recognises a need for better understanding of how beliefs and trust shape people’s engagement with pathways in the NHS.
In this report we summarise the findings of a research and co-design project, undertaken between May 2024 and February 2025, to:
- Understand belief and trust barriers to engaging with digital health services
- Develop a simple resource as a first step to addressing these barriers.
Defining 'digital health services'back to top
We adopted a broad definition of ‘digital health services’ to include a range of digital platforms, apps and tools that are commonly used within the NHS for different types of interaction, including:
- Online appointment booking platforms
- The NHS App for managing appointments, prescriptions and health information
- Video platforms for consultations or receiving therapy
- Other apps and devices for monitoring health conditions and symptoms or receiving therapy
- Other online platforms for accessing medical notes.
Our main focus for the project was primary care (in the UK), as this is where most people will first encounter digital health tools and services. However, in our approach, we welcomed perspectives from beyond primary care settings.
Belief and trust barriers: what the evidence tells usback to top
Our rapid review of evidence, conducted in May and June 2024, surfaced a range of beliefs and concerns around using digital health services. The evidence also shows overlap between the groups of people more likely to lack trust in using digital health services and groups who experience more health and healthcare inequalities⁴. A summary of the review findings is presented below; the full review is available on the Good Things Foundation website⁵.
Patient / public beliefs about digital health servicesback to top
Concerns about communication challenges, leading to poorer care
- Belief that it is harder to build connections and / or communicate fully about health concerns via digital tools such as appointment booking platforms, or video consultations, leading to inappropriate or delayed care.
Concerns about getting it wrong, leading to not getting the right care
- Belief that it is easier to make a mistake using digital tools when inputting or sharing information, which could lead to not getting the right care at the right time.
Concerns about an increased burden of care for some
- Belief that increased use of digital health services, such as virtual wards, will place more responsibility onto patients and / or carers, with potential for poorer quality care.
Patient / public trust concerns around digital health servicesback to top
Lack of trust in how personal data will be stored and protected digitally
- Lack of trust and understanding about how data is shared through digital health services, who has access to data and the risk of data breaches.
Lack of trust in the accuracy of data being collected and used digitally
- Concerns that data collected through digital health services may not accurately reflect people’s lived experiences and / or may not reflect diversity of identities, leading to inappropriate decisions about care.
Lack of trust in how digital services are being rolled out
- Perception that increasing digital health services is a cost-cutting exercise, leading to poorer access to care.
Groups most likely to experience trust concernsback to top
- People with disabilities have lower levels of trust in the NHS
- People from lower social grades have lower levels of trust in how data is protected
- People from minority ethnic groups have lower levels of trust in how data is protected, and have more concerns about their data being used to discriminate against them
- People who experience vulnerabilities have lower levels of trust around accessing care and data sharing, e.g. people experiencing homelessness; refugees / asylum seekers; Gypsy, Roma and Traveller communities; sex workers
- Unpaid carers may face or perceive additional burdens around accessing care through digital.
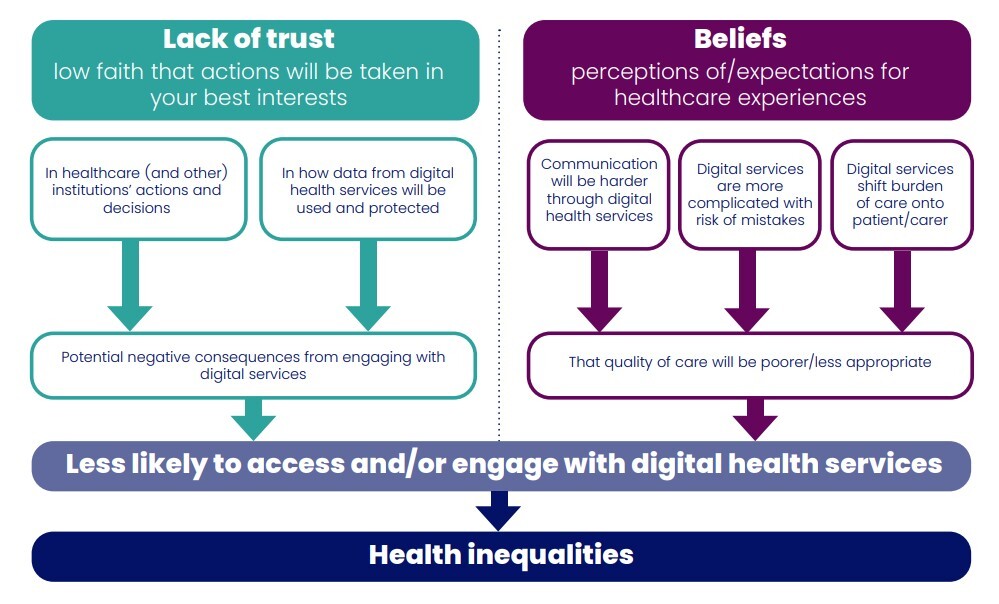
Conceptualising the link between belief and trust barriers, and health inequalitiesback to top
The insights from the evidence review informed our creation of a conceptual framework (below). We used this framework to inform a co-design approach to develop a simple resource to help address belief and trust barriers to using digital health services.
Co-designing a resource to address belief and trust barriersback to top
Our approachback to top
Drawing from the Double Diamond design framework⁶, we developed a three-stage process to co-design a resource to address belief and trust concerns around digital health services. We worked with people with experience of facing challenges to do things online, plus consulted with healthcare staff and other communities. Our approach included:
- Discover and Define - October 2024 - In-person workshops, hosted by community organisations, with 32 people with lived experience: Explored experience, beliefs and concerns around digital health services.
- Design - November 2024 - January 2025 - In-person workshops with 27 of the 32 participants from the first round of workshops: generated ideas for a resource to address priority concerns.Online consultation sessions and survey with 19 healthcare staff and community members: elicited feedback on draft structure and content for the resource, and how to maximise engagement.
- Refine and Deliver - February - March 2025 - Further feedback via phone and email from 17 participants from the community workshops to refine the draft resource.
Belief and trust barriers: insights from people with lived experienceback to top
People with experience of challenges doing things online identified a range of belief and trust barriers to engaging with digital health services, as well as some positive experiences:
- Lack of trust around privacy and data sharing
- Perception that care through digital health services may be of poorer quality
- Perception that digital health services might be difficult to use
- Concern about a lack of choice and autonomy
- Positive engagement with digital health services.
Key learningback to top
These belief and trust barriers may pose more of a challenge for people with language, literacy or communication challenges, those with limited digital skills, and people with caring responsibilities. However, examples of positive engagements with digital health services highlight value in helping address belief and trust concerns.
Lack of trust around privacy and data sharing back to top
“Who is accessing my medical notes? We are not told”
There is confusion and anxiety about who can access personal data through digital health services. People feel uncertain about how data is collected and stored, and they worry that it might be shared with people beyond the health service without their knowledge, e.g. employers.
“Scams!”
Much of the uncertainty in how data is stored reflects people’s wider fears of online scams, data hacking and identity theft. This comes from personal experience as well as from broader narratives such as reports of high level data breaches in and beyond the health services.
“Not [safe] when I am outside”
The accessibility of digital health services also raises concerns about confidentiality and privacy when using these services in different places. For example, people feel more at risk of data hacking if using the NHS App on a phone whilst in a public place. They can also be concerned about a lack of privacy in the home for video consultations, something that might particularly affect people living in crowded or insecure accommodation.
Care through digital health services may be of poorer quality back to top
“Sympathy is not there”
People are concerned that care provided through digital health services lacks a personal touch, and might be less responsive to a patient’s needs. For example, when receiving mental health support through an app, there is a sense of it lacking someone who really ‘cares’ about the patient’s wellbeing.
“Don’t see me”
Many people are concerned about it being more difficult to communicate information about health and symptoms effectively through appointment booking platforms, and that important, non-verbal ‘clues’ can be lost through video consultations. People feel this might lead to not receiving appropriate diagnosis or care for their condition. There is a fear that people with learning disabilities and communication challenges, such as limited English, might be more disadvantaged.
Case exampleback to top
One workshop participant described an experience of her grandchild’s condition being ‘misdiagnosed’ via video consultation, leading to them requiring hospitalisation. She felt she would be unable to ‘trust’ remote consultations again.
“Asks for too much information”
Some people worry that you need to be ‘intelligent’ to be able to describe symptoms effectively through a digital platform, for example, when requesting an appointment at a GP practice. It can be overwhelming to be required to provide lots of written detail, made more difficult for some by dyslexia, literacy difficulties or poor mental health. They feel this risks not receiving appropriate care for their condition, or access to care being delayed.
Case exampleback to top
A participant with English as a second language stated they are confident in speaking English but less confident with writing. They are reluctant to use online appointment platforms since an incident trying to describe feeling dizzy, but a translation tool translated ‘dizzy’ to the word ‘stoned’.
Harder to be taken seriously
A few participants expressed concern that interactions through digital platforms could make it harder to challenge or question a diagnosis or decision about care. They felt it would be more difficult to ask for a second opinion if they felt unhappy with a consultation or outcome. This concern seems to reflect a broader perception that digital health services lack the personal connection and accountability that is associated with face-to-face care.
Digital health services might be difficult to useback to top
“Try again tomorrow”
People are concerned about a lack of information and support provided around using digital health services, and some feel that the platforms and apps are designed for ‘younger people’. Many don’t know where to turn to ask for support if a digital service doesn’t seem to be working, for example when repeatedly receiving a message on a platform to ‘try again tomorrow’.
“Another thing to worry about”
People less confident about their digital skills worry that getting started with a digital health service will be complicated and time-consuming. This could create additional stress, especially when people are feeling unwell or anxious about their health, and could create an additional burden for carers.
“How do I know it gets it right?”
People are worried that there is a higher chance of mistakes being made through digital health services, either by themselves or by healthcare staff, with potential impacts on access to the right care at the right time, such as accessing prescriptions. People have experienced digital tools being ‘glitchy’, for example data being ‘lost’ or ‘hidden’ in the NHS App, and feel uncertain about how to resolve these issues.
Concern about lack of choice and autonomyback to top
“There is no turning back”
People feel they have limited choice in how they can access health services through digital and worry that once you accept a digital service, there is no option to return to in-person services. There is doubt around whether hybrid models of in-person and digital health services are available.
Not patient-centred
The roll-out of digital health services are seen to be a cost-cutting strategy, rather than to improve access to care. People feel they lack control over how services are being made available and that digital services are not being designed for people ‘like them’, who may lack digital confidence or struggle with English.
Positive engagement with digital health servicesback to top
Experiences with digital health services can be positive, and are valued by some for:
- Convenience: Being able to make appointments online can save time and be done on the move
- Accessibility: Being able to access online services outside of normal working hours is useful for managing time amid busy schedules, e.g. for carers
- Choice: A ‘pick and mix’ approach to accessing care through digital and non-digital services, depending on preference
- Access to information: Accessing personal information about care and conditions can be easier through digital services such as the NHS App
- Friendly support: Receiving help from staff to register and start using digital services can make all the difference.
Designing a resource to address belief and trust barriersback to top
Co-designing a resource to address barriers to using digital health services involved exploring ideas for the content, form and design of the resource, as well as considering the context in which the resource would be best used.
What the resource should coverback to top
- Information on privacy and data security: Simple explanations about data storage and ownership; how to tell if a digital message from the NHS is genuine; explanations of how digital services are safe to use
- Step-by-step guidance on using digital services: Aimple information about how to access and use common digital platforms, such as the NHS App; a ‘digital health services for dummies’ guide
- Troubleshooting information: Frequently asked questions and tips for addressing common problems encountered in digital health services; demystifying concerns about making a mistake on a digital platform
- Examples of successful use: Case studies of how people have engaged successfully with digital health services, or how they have overcome issues or concerns about using them; the benefits of using digital health services
- Reassurance: Guidance on asking questions about digital health services to get more information and support; reassurance about being able to choose between digital and traditional health services
- Signposting: Providing links to trusted, existing information sources.
The form and design of a resourceback to top
- Balanced tone: There needs to be recognition of the benefits and challenges of using digital health services, and to not appear to be ‘selling’ digital health services
- Simple, but not condescending language: Easy to follow, plain language, with good balance of text and visuals, without being overly simplistic or condescending
- Visual design: Visuals to illustrate step-by-step process, eg of using a digital health service
- Space for notes: Including space for people to annotate and record their own notes in relation to using digital health services or accessing more information
- Booklet-style leaflet for a physical resource: Eye-catching and easy to pick up; wallet-sized resource was considered to be too small and ‘fiddly’
- Available in alternative formats: Short videos or animations with subtitles; interactive online guide with clickable links; a Facebook group for sharing information.
Using the resource in context back to top
- Accessible for everyone: Available and accessible in multiple places including community centres and libraries, as well as healthcare settings
- To be used in conversation: More effective if used as part of a conversation between a patient and a health or community worker, to encourage questions and dialogue
- Embed within other initiatives and interactions: Such as community health events, registration processes at GP practices, and in consultations
- Use it to initiate wider dialogue: Use the resource to encourage conversation and sharing of experience between people, for example in workshops or peer support events, to help increase knowledge and confidence.
Further considerations for designing a resourceback to top
- Ensuring information is relevant and up-to-date: With variability across the health system in the type of digital health services available, the information must be relevant to different audiences, and links kept up-to-date
- Ensuring the resource is easy to print: It needs to be designed to be printed easily in community settings
- Producing the resource in different accessible formats: Such as in Easy Read, different community languages and an audio format
- Creating an online version to help build digital confidence: A simple, interactive online resource could be valuable for helping people practice and build their confidence around using digital tools.
Wider learning for inclusive digital health servicesback to top
The project generated further insights around the accessibility of digital health services, beyond the scope of the resource to address belief and trust barriers.
- Poor user interface and experience: Digital health service platforms are often not designed with diverse users in mind. Complex interfaces and confusing navigation can discourage both patients and staff, and may not be accessible for people with language, literacy or other needs
- Too much variety in digital tools: The wide range of platforms and apps used across the health service and the lack of consistency between them, can make it challenging for patients and staff to navigate digital services confidently
- Lack of confidence, time and support among staff: Healthcare staff can also lack confidence in using digital health tools, and may lack capacity to answer questions and provide support to patients around digital health services
- The reasons for the digital shift should be better communicated: The health system and its staff are not always very good at explaining how the move towards digital services is designed to improve access to care, rather than just be cost-saving.
Putting our learning into actionback to top
Belief and trust barriers to engaging with digital health services centre on concerns about risks to personal data; concerns about delayed or poor quality care due to communication challenges or making a mistake; and concerns about a lack of choice about how to engage with health services.
However, there is also openness to learning more about digital health services and the benefits they can bring to people’s access to care. Accommodating ideas generated through the co-design process, we have developed a simple, off-line resource to help people feel:
- Reassured: That others have similar concerns about and frustrations with using digital health services; but that personal data is secure and that there are benefits to using them
- Confident: To ask questions about their concerns with using digital health services; to ask for support with using digital tools and platforms; and to request alternative approaches to accessing care when appropriate.
The resource should be seen as a first step. It is our intention to develop further, accessible versions of the resource, with appropriate funding.
Recommendations for further workback to top
From our learning through this project, we recommend the following actions for developing wider support to ensure digital health services are accessible and inclusive for all:
- Explore barriers faced by healthcare staff in i) using different digital health services and platforms, and ii) supporting patients and service users to engage with these services. Healthcare staff need to be empowered to support patients, answer their questions and address their concerns.
- Embed inclusive design approaches into the design of new digital health services. New services should be designed with involvement of people with lived experience of digital exclusion to ensure they are accessible and inclusive for people facing different digital barriers⁷. Where possible, the development of new digital tools should be minimised, to help reduce the variety of platforms and tools patients and staff are required to navigate.
- Strengthen local support provision. Funding and capacity-building are needed to ensure that there is equitable local support available for using digital health services at the point at which people need help. This could be provided within GP practices, community centres and other local spaces. Simple, online support and troubleshooting could be a valuable addition to in-person support.
- Transparent communication. Develop clear, consistent messaging around the benefits and security of digital health services, while acknowledging their current limitations, to help bridge the trust gap.
Resource to address concerns about digital health servicesback to top
The resource titled “Worried about using digital health services?”, is an eight-page, A5 sized leaflet, designed to be easily printed in colour or black and white. It covers four themed sections of concern around digital health services (data security, communication, challenges using digital tools, choice). These sections include suggestions of questions people can ask to explore their concerns, short case studies of experience of these barriers, and signposting to further information.
We have designed the resource to be used in community and healthcare settings, to prompt conversation about using digital health services, and to empower people to ask questions to explore if digital services are suitable for them. It is also designed to signpost people to further resources around digital health services, and building digital skills and confidence more generally.
Acknowledgementsback to top
We gratefully acknowledge the collaboration and contributions of all the participants of the co-design workshops; the three community organisations who hosted with co-design workshops; the participants of the consultation activities; NHS England’s National Healthcare Inequalities Improvement Programme; and member organisations of the VCSE Health & Wellbeing Alliance. We gratefully acknowledge funding provided through the VCSE Health & Wellbeing Alliance.
Footnotes and notesback to top
Footnotes
¹ Good Things Foundation (2024). Digital inclusion and health - summary of key statistics
² Lloyds Bank (2023). 2023 Consumer Digital Index
³ NHS England (2024) Inclusive digital healthcare: a framework for NHS action on digital inclusion
⁴ Kings Fund (2022). What are health inequalities?
⁵ Good Things Foundation (2025). Beliefs and trust barriers to engaging with digital health services: a literature review.
⁶ The Design Council. 2003. “The Double Diamond”. https://www.designcouncil.org.uk/our-resources/the-double-diamond/
⁷ For guidance on designing digitally inclusive services in general practice, see Good Things Foundation (2022). “Top tips: supporting digital inclusion in practice”
Notes
A more detailed description of the project methodology and participants is available on request from Good Things Foundation.
We also encourage the resource to be shared widely across community and health networks, and welcome feedback on its use.
Questions and feedback can be sent to: research@goodthingsfoundation.org.

